By R. Scott Nolen and Malinda Larkin
As the epizootic of highly pathogenic avian influenza (HPAI, more specifically avian influenza type A H5N1) spreading globally approaches its fourth year, animal and public health officials are monitoring how quickly a new variant of the H5N1 virus—the clade 2.3.4.4b viruses—can jump to new animals, including people.
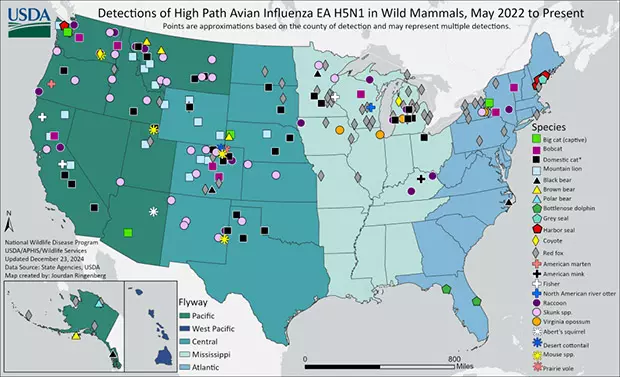
Given H5N1's circulation among wild and migratory bird populations, along with clade 2.3.4.4b's knack for infecting a broad range of mammalians species and the associated morbidity and mortality rates, experts worry H5N1 will eventually mutate into a lethal strain capable of human-to-human transmission, setting off another pandemic.
However, as the Centers for Disease Control and Prevention (CDC) reports, the current risk to individual and population health remains low and has not significantly changed from the most recent assessment done on a similar H5N1 virus that caused an outbreak among mink in 2023 in Spain.
That said, the virus strain found in dairy cows in the U.S. may only need one mutation for it to be able to spread among humans, according to a study published in the journal Science in early December.
"The longer this virus circulates unchecked, the higher the likelihood it will acquire the mutations needed to cause a pandemic. We need to act urgently to prevent this scenario," warned Dr. Les Sims, who has worked in Asia and internationally for over 30 years on the prevention and control of major infectious diseases of food-producing animals.
Backyard pigs
Noncommercial pigs on a mixed-species farm in Crook County, Oregon, are the latest livestock species found to be infected by the H5N1 2.3.4.4b viral clade.
In late October, the Oregon Department of Agriculture diagnosed H5N1 in poultry on the affected farm. Days later, the U.S. Department of Agriculture (USDA) confirmed the virus in two of five pigs on the farm marking the nation's first reported H5N1 swine infection during the current epizootic.
Genomic sequencing indicated that both the infected poultry and swine harbored the D1.2 genotype of H5N1. Similar sequences were found in local migratory birds, suggesting that the farm animals likely contracted the virus through contact with these birds, rather than from other livestock. In short, a new introduction rather than lateral transfer.
During a November 20 media call, Dr. Ryan Scholz, the Oregon state veterinarian, said the farm's setup—where poultry and swine shared water sources, housing, and equipment—may have facilitated interspecies transmission. One pig was seen eating a dead duck prior to the outbreak, he added.
Out of an abundance of caution, all five pigs were sedated then euthanized, Dr. Scholz said.
While U.S. swine producers have kept H5N1 at bay so far, the fact that the pigs on the Oregon farm had been infected is troubling when considering how an HPAI pandemic might begin, experts say.
During the call with reporters, Dr. Montserrat Torremorell, professor and chair of the Department of Veterinary Population Medicine at the University of Minnesota College of Veterinary Medicine, described pigs as "mixing vessels" for influenza viruses, specifically those infecting birds, humans, and other pigs. If the H5N1 2.3.4.4b clade were to become endemic in U.S. pigs, then those viruses could undergo genetic reassortment, creating entirely novel strains.
"What would happen in that case, it's really an unknown, but it's something we're concerned with," Dr. Torremorell said. "Those new reassorted viruses would have increased virulence, increased transmissibility among other species, and represent a higher risk to people. So that's something … that we would have to keep an eye on."
Dr. Abbey Cannon, director of public health and communications for the American Association of Swine Veterinarians, told AVMA News that the swine industry has a robust influenza surveillance program that monitors endemic, emerging, and novel influenza strains affecting swine.
Since 2009, U.S. pork producers and swine veterinarians have actively participated in the USDA's swine influenza surveillance program to enhance animal and public health by sharing crucial information with the CDC and animal and public health officials, she added.
"The swine influenza surveillance program is designed to identify influenza viruses circulating in swine, proactively detect reassortment viruses that could impact public health, and gain knowledge to contribute to improved animal health diagnostics and vaccines," Dr. Cannon said.
Epizootic
While the U.S. swine industry remains untouched by H5N1, the virus continues to infect commercial poultry and dairy cattle operations across multiple states, including some of the farm workers and others.
The virus was initially detected in wild birds in Newfoundland and Labrador, Canada, in December 2021. The following month, the first wild birds were diagnosed with the highly pathogenic virus, then the first commercial poultry facility in February 2022. Since then, the USDA says H5N1 outbreaks have been detected in all 50 states—1,324 commercial flocks and 729 backyard flocks—resulting in the depopulation of more than 125 million turkeys and chickens. There have also been 10,852 positive wild bird samples. In late November, H5N1 was detected for the first time in Hawaii at a bird sanctuary.
Dairy milk producers, veterinarians, and government officials have been struggling to contain H5N1's spread among dairy cattle since the virus was first detected in a Texas herd this past March. As of late December, H5N1 had been confirmed in more than 901 dairy cattle herds in 16 states, most recently Michigan and Utah, but also in California, Texas, Kansas, Idaho, New Mexico, Ohio, Michigan, South Dakota, North Carolina, Colorado, Minnesota, Wyoming, Oklahoma, and Iowa.
California declared a state of emergency on December 18 with Gov. Gavin Newsom citing the recent discovery of H5N1 cases in Southern California dairy herds as the impetus, signaling the need to expand monitoring and build on the coordinated statewide approach to containing and mitigating the spread of the virus. California is the nation's top milk-producing state with more than 1,100 dairy farms housing 1.72 million milk cows.
According to the California Department of Food and Agriculture, "Bird flu virus levels have been demonstrated to be high in raw milk from infected cows, and sporadic human cases identified in workers in close contact with infected dairy cows and their milk indicate that raw milk is infectious to humans."
Since April, the CDC has confirmed H5N1 clade 2.3.4.4b infections in 64 people in the United States. Twenty-two of these cases were associated with exposure to infected poultry, 39 were associated with exposure to infected dairy cows, and two sources of infection remain unknown with potential exposure to other animals such as backyard flocks, wild birds, or other mammals.
A notable case involves a child in California, marking the first reported instance of H5N1 in a U.S. minor. The child exhibited mild symptoms and is currently recovering, the CDC says. Investigations are ongoing to determine the exact source of infection, with potential links to exposure to wild birds.
More recently, the CDC announced on December 18 the first severe case of H5N1 in the U.S. That patient had been exposed to sick and deceased birds in backyard flocks. After conducting a genetic analysis, the CDC "identified low frequency mutations in the hemagglutinin gene of a sample sequenced from the patient, which were not found in virus sequences from poultry samples collected on the patient’s property, suggesting the changes emerged in the patient after infection."
Person-to-person spread of the virus has not been reported. Generally, cases have been mild in humans. In a study that looked at 1,288 Michigan residents who were monitored for signs and symptoms after potential H5N1 virus exposure, 53 (4.1%) reported signs and symptoms, 52 of whom received testing for influenza A(H5). Two dairy workers received positive test results (3.8% of all persons tested), which was less than 1% of all monitored dairy workers, according to the findings published in the July 25 edition of the Morbidity and Mortality Weekly Report.
Biosecurity
The USDA and FDA, along with the CDC, are collaborating to monitor and control the spread of H5N1. Efforts include enhanced surveillance of poultry and livestock, culling of infected flocks, indemnity and compensation for producers that have sustained losses related to H5N1, and public health advisories to minimize human exposure.
The USDA's Animal and Plant Health Inspection Service (APHIS) issued an announcement on December 13 reminding all animal caretakers of the importance of biosecurity for all animal facilities and farms.
Animals can be exposed to H5N1 through various pathways, including the consumption of infected birds or other animals, and unpasteurized milk from infected cows. Many species are susceptible to influenza viruses. Felines, including both domestic and wild cats, such as tigers and mountain lions, are particularly sensitive to avian influenza and care should be taken to not expose these animals to the virus, according to the FDA.
Dr. Angela Demaree, immediate past president of the American Association of Food Safety and Public Health Veterinarians, says her organization is urging cat owners to stop feeding raw diets and transition to high-quality canned cat foods. In addition to concerns about H5N1, raw diets may also contain zoonotic bacteria such as Salmonella or Campylobacter.
"Additionally, we are reminding cat owners that if they visit farms or interact with chickens or livestock to practice good biosecurity by cleaning and disinfecting shoes, changing clothes, and washing hands before greeting their feline friends."
According to the USDA, "Biosecurity continues to be the best weapon against the spread of H5N1 to any susceptible species. Data collected since March 2024 has shown that H5N1 can be transmitted on equipment, people, or other items that move from place to place. All facilities should practice good biosecurity even if the virus has not been detected in their state or vicinity, this includes following proper cleaning and disinfecting procedures and infection control practices."
In addition, the CDC says continued monitoring for clinical signs of disease and testing are critical to finding genetic or epidemiological changes that might alter the risk assessment.
Vaccination
The complexity of H5N1 outbreaks requires a coordinated, One Health response that integrates animal health, human health, and environmental stewardship, according to Dr. Sims. He is a veterinary consultant and former assistant director of the Agriculture, Fisheries and Conservation Department for the Hong Kong Special Administrative Region Government.
He advocated for continued and stepped-up research to fill in knowledge gaps, such as transmission pathways, host adaptation, and environmental stability, as well monitoring of wild bird populations, poultry farms, and high-risk mammalian hosts.
"The virus has fundamentally changed the way we need to think about managing avian influenza," Dr. Sims told AVMA News. "It's no longer a question of sporadic outbreaks but of persistent, multispecies infection cycles that threaten both human and animal health."
Dr. Sims said H5N1 vaccination in poultry is a critical tool against the virus but recognizes using such vaccines is limited in the United States due to concerns about trade restrictions. Dr. Sims continued. "Vaccination can dramatically reduce infection rates in poultry, prevent wildlife spillovers, and ultimately safeguard human health," said Dr. Sims, adding that HPAI vaccination programs have been successful in Hong Kong and Vietnam.
Click here to see more...